Introduction
Pain management has been designated as ‘a human right’ by international organizations (1, 2) but one hundred million adults in the U.S. have chronic pain (3). This statistic is greater than the number of individuals affected by diabetes, cancer, and heart disease combined (3, 4). The prevalence of persistent pain also increases with age, with rates as high as 65% among community-dwelling seniors and 80% among seniors living in long-term-care facilities (5). The situation is no better among Canadian children and adolescents; like adults, one in five suffer persistent forms of pain, with an estimated 5% to 8% enduring pain that is severe enough to interfere with school work, social development, and physical activity (6, 7). Chronic pain is costly not only to the patient but also to society as a whole. Expenditures on chronic pain include both direct costs related to treatment and provision of health care services, and indirect costs such as those associated with loss of productivity, lost tax revenues and disability payments. Health care costs for Canada at more than $6 billion per year, and productivity costs related to job loss and sick days at $37 billion per year (8, 9). One in five Canadian adults report persistent pain that imposes significant activity limitation, difficulty at work, and financial hardship due to increased reliance on health services not covered by public health-insurance plans (10, 11). In the meantime, chronic pain is associated with the worst quality of life compared with other chronic diseases such as chronic lung or heart disease (9). It doubles the risk of suicide in chronic pain patients compared with people without chronic pain (12) and a sense of hopelessness (13), and suicide rates remain higher even when controlling for mental illness (14). Although pain education has been identified as a strategy to improve ineffective pain management practices (15), recent evidence supports the continuing lack of pain contents in health science curricula, particularly for prelicensure students in Canada as in other countries (16-18). Despite evidence that well-designed pain curricula can significantly improve pain knowledge and beliefs of health professional students (19-21). Attitudes and beliefs reinforced as undergraduates are more difficult to change later (22) reports of pain content in prelicensure (prequalifying, preregistration) curricula are minimal.
Prelicensure environment
In Canada the length of nursing programs varied from two to four years but there are only five studies in literature examining pain knowledge in prelicensure environment and focus on palliative care or specialty populations (18, 23-26). A recent Pain Education Survey described the time for mandatory pain content taught in the curricula of the ten major Canadian universities in health science programs like dentistry, medicine, nursing, occupational therapy, pharmacy and physical therapy (17). Over 90% of the health science programs stated they included mandatory formal pain content in the curriculum but the majority (67,5%) were unable to specify designated hours for pain program because they had ‘integrated content’ across several courses and/or clinical conference (only 5.5% as a separate course or content). The average total time designated for formal pain teaching over the entire academic training program within Nursing Faculties was 31 hours (SD +-42; range 0-109). Except for physical therapy, the mean total number of hours designated within Nursing Faculties was higher than the other disciplines (15 dentistry, 16 medicine, 28 occupational therapy and 13 pharmacy). All respondents commented that pain education was also addressed in clinical placements, although most respondents were unable to estimate the duration and indicated that it was variable, depending on the particular clinical placement (eg palliative care and pain clinic). Respondents were also asked to categorize the pain content covered in their curriculum into eight specific areas (neurophysiology mechanisms, etiology and prevalence, misbeliefs and barriers, assessment and measurement, management: analgesics and adverse effects, management non-pharmacological, multidimensional nature of pain, monitoring and quality improvement policy/guidelines) and estimate the percentage’s time spent teaching each category. All health science programs covered each specific area but in different percentages of time. For example, the percentage for assessment and measurement of pain were 13% for nursing and 7% for medicine. Conversely, pharmacological pain management were higher for physicians (25%) than for nurses (12%).
Similar things are found from a survey that identified and prioritized the educational needs of 72 health care providers (9 physicians, 3 pharmacists, 6 physical therapists, 9 occupational therapists, 21 orderlies and 24 nurses) working in long-term care facilities with regard to pain management in Quebec (27). Physicians and pharmacists requested more information about drug interactions, management of adverse effects, best treatment strategies for neuropathic pain (eg. coanalgesics, topical analgesics), progression and substitution of pharmacological agents (eg. indications and principles of prescription). In the other side, nurses requested more information about how to determine when nonspecific pain behaviors, such as crying or agitation, were related to pain or to another problem (eg. depression, loneliness) or how to recognize the specific clinical signs and symptoms of pain, especially in patients unable to communicate or patients with dementia. However, the educational need for pain assessment and communication issues within multidisciplinary teams were very highly ranked in each health care providers because they wanted to know the specific roles of each health care provider involved in patient care and the best strategies to effectively communicate pain-related information.
Pain competency statements were found only for nursing and dentistry in a entry-to-practice competency requirements related to pain knowledge, skill and judgment examined in Canadian national, provincial and territorial documents for seven health professions (dentistry, medicine, nursing, pharmacy, occupational therapy, physiotherapy and psychology) (28). No references to competencies related to pain knowledge, assessment or management were found in the remaining health science documents. In particular, Nursing included a total of nine specific national pain competencies related to pain assessment and two nonspecific pain competencies related to palliative and/or end-of-life care needs (Table 1).

For almost 20 years the International Association for the Study of Pain (IASP) has recognized the need to facilitate educational initiatives. Finally, in 2012 the IASP has established coordinated curriculum guidelines for individual professions including Nursing (29). These competencies represent the expectation of minimal capabilities for graduating nursing students for pain management and within each of the 4 domains there are the principal values of nursing such as advocacy, collaboration, compassion, effective communication, empathy, patient-centered care, interprofessional teamwork, comprehensive care, ethical treatment, cultural inclusiveness and evidence-based practice.
University of Toronto: A mandatory 20-h Interfaculty Pain Curriculum
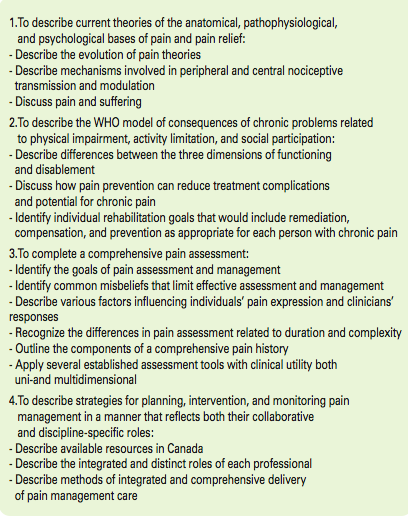
Since 2002 the Education Advisory Committee of the University of Toronto Centre for the Study of Pain (UTCSP) proposed to provide one integrated course to all undergraduate students in the Health Science Faculties (Dentistry, Medicine, Nursing, Pharmacy, Physical Therapy and Occupational Therapy) (20). The aim was to ensure a common basic understanding of pain assessment and management principles upon which to build profession-specific pain knowledge within an interprofessional context. Consequently the professionals could understand each other better and value what each brings to collaborative practice (30). Documentation of elective shared educational courses for Canadian Health Science students was reported over 30 years ago (31, 32). The pain curricula for this integrated course was created by surveying all pain curricula currently being taught within the six participating professional programs to determine the baseline requirements, the core and discipline-specific pain curricula from IASP and the Position Statement on Pain Relief from the Canadian Pain Society (33) from which we formulated the objectives to guide the content development as outlined in Table 2.
Currently, Tte UTCSP–Interfaculty Pain Curriculum continues to bring together students from six health sciences faculties (in 2014, a total of 947 students) to take part in a mandatory 20-hours curriculum targeting pain misbeliefs and optimal interprofessional pain assessment, care planning, and management practices.
In the last years a new approach to bridge the gaps of knowledge about pain there was the creation of a web-based Pain Education Interprofessional Resource (PEIR) for prelicensure health science students for use in universities across Canada (38). The PEIR has been designed using a model of scaffolded knowledge building to support individual web-based learning, with flexible extensions to enable interprofessional student, expert-facilitated, online and/or face-to-face discourse.
Postlicensure environment
By more than four decades the master’s program of Schools of Nursing in Canada offer tailored programs in Advanced Nursing Practice (ANP) and prepared students for Clinical Nurse Specialists (CNSs) or Nurse Practitioners (NPs) roles in selected fields as nursing administration, nursing education, global health or in specialized area of nursing like Primary Health Care, Family Care, Critical Care, Neonatal Nursing, Anesthesia Care, Oncology (34).
The Canadian Nurses Association (CNA) recognizes the acquisition of competencies in pain for ANP through experience and education programs, but there isn’t specialized master about pain. However two thirds nurses working in Acute Pain Service throughout Canada have a master’s prepared in a specialized area of nursing (35).
The core competencies in pain management
In 2012, starting from the guidelines for pain education published by the IASP (37), an interprofessional group of North American pain experts participated in a consensus project to develop core competencies in pain management for pre-licensure clinical education that can serve as a foundation for the development of comprehensive pain management curricula across all health professions (36). After that an executive committee synthesized current evidence and 30 members representing 10 professions (dentistry, medicine, nursing, pharmacy, physical and occupational therapy, psychology, social work, alternative and complementary medicine and veterinary medicine) recommend a set of consensus-based competence, a final work of domains and competencies was completed (Table 3).

For Canada, this work is an important contribution to ensuring competence in essential knowledge and skills to provide effective pain management on graduation. This curriculum now provides a means for Faculties of Nursing to learn a common language and to develop a basic understanding of pain mechanisms and biospsychosocial concepts fundamental to competent practice, grounded in the recognition of adequate pain relief as a fundamental human right. The next step is to encourage the inclusion of these domains and competencies in professional accreditation and licensure requirements for all universities of Canada.
Conclusion
The continuing high prevalence of pain, both acute and persistent, is a public health problem. Embedding pain management core competencies into prelicensure nursing education is crucial to ensure that nurses have the essential knowledge and skills to effectively manage pain and to serve as a foundation on which clinical practice skills can be later honed.
In Canada, despite the availability of internationally accepted core and discipline-specific curricula, the majority of health science faculties and departments found it difficult to delineate the actual hours allotted to teaching pain content in their curriculum. Moreover pain education was also addressed in clinical placements and, as a result, it varied among students, depending on their particular clinical experiences and clinicians involved (17).
In 2010 the International Association for the Study of Pain (IASP) hosted the first International Pain Summit, in Montreal, Quebec. More than 250 representatives from 84 countries, and professional and human rights organizations endorsed that access to pain management is a fundamental human right and contributed to the Declaration of Montreal. The declaration recognized the intrinsic dignity of all persons and the right of access to pain management without discrimination. Two years later, IASP has established coordinated curriculum guidelines for individual professions including Nursing.
The Canadian Nurse Association recommend providing a pain-theories course with clinical application for all levels of nursing education, both undergraduate and graduate because it is essential that Canada takes a leading role in embracing the Declaration of Montreal and shows that it is possible to treat Canadian citizens with the compassion and dignity that they deserve.
Bibliografia
- Brennan F, Carr DB, Cousins M. Pain management: a fundamental human right. Anesth Analg 2007; 105(1): 205-21
- Lynch ME.,The need for a Canadian pain strategy. Pain Res Manag 2011; 16(2): 77-80
- Committee on Advancing Pain Research, and Education, Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: Institute of Medicine of the National Academies, 2011
- Gaskin D, Richard P. The economic costs of pain in the United States. J Pain 2012; 13(8): 715-24
- Hadjistavropoulos, T, et al. Transforming long-term care pain management in north america: the policy-clinical interface. Pain Med 2009; 10(3): 506-20
- Huguet A, Miro J. The severity of chronic pediatric pain: an epidemiological study. J Pain 2008; 9(3): 226-36.
- Stanford EA, et al. The frequency, trajectories and predictors of adolescent recurrent pain: a population-based approach. Pain 2008; 138(1): 11-21
- Phillips CJ, Schopflocher D. The Economics of Chronic Pain, in Chronic Pain: A Health Policy Perspective. Weinheim: Wiley, 2008
- Choiniere M, et al. The Canadian STOP-PAIN project – Part 1: Who are the patients on the waitlists of multidisciplinary pain treatment facilities? Can J Anaesth 2010; 57(6): p. 539-48
- Moulin DE, et al. Chronic pain in Canada–prevalence, treatment, impact and the role of opioid analgesia. Pain Res Manag 2002; 7(4): 179-84
- Schopflocher D, Taenzer P, Jovey R. The prevalence of chronic pain in Canada. Pain Res Manag, 2011; 16(6): 445-50
- Tang NK, Crane C. Suicidality in chronic pain: a review of the prevalence, risk factors and psychological links. Psychol Med, 2006; 36(5): 575-86
- Fishbain DA, et al. Completed suicide in chronic pain. Clin J Pain, 1991. 7(1): p. 29-36.
- Ratcliffe GE, et al. Chronic pain conditions and suicidal ideation and suicide attempts: an epidemiologic perspective. Clin J Pain, 2008; 24(3): 204-10
- Sessle, B. Incoming president’s address: looking back, looking forward. In: Devor M, Rowbotham MC, Wisenfield-Hallin Z, editors. Progress in pain research and management. Proceedings of the 9th World Congress on Pain; 1999 Aug 22–27; Vienna, Austria. Seattle: IASP Press; 2000: 9-18
- Simpson, K, Kautzman L, Dodd S. The effects of a pain management education program on the knowledge level and attitudes of clinical staff. Pain Manag Nurs 2002; 3(3): 87-93
- Watt-Watson, J, et al., A survey of prelicensure pain curricula in health science faculties in Canadian universities. Pain Res Manag, 2009; 14(6): 439-44
- Briggs EV, Carr EC, Whittaker MS. Survey of undergraduate pain curricula for healthcare professionals in the United Kingdom. Eur J Pain, 2011; 15(8): 789-95
- Wilson JF et al. Medical students’ attitudes toward pain before and after a brief course on pain. Pain, 1992; 50(3): 251-6
- Watt-Watson J et al. An integrated undergraduate pain curriculum, based on IASP curricula, for six health science faculties. Pain, 2004; 110(1-2): 140-8
- Leila, NM et al. Training medical students to manage a chronic pain patient: both knowledge and communication skills are needed. Eur J Pain, 2006; 10(2): 167-70
- Barr H, et al. The evidence base and recommendations for interprofessional education in health and social care. J Interprof Care, 2006; 20(1): 75-8
- Plaisance L, Logan C. Nursing students’ knowledge and attitudes regarding pain. Pain Manag Nurs, 2006; 7(4): 167-75
- Samuels JG, Leveille DM. Senior nursing students’ clinical judgments in pain management. Nurse Educ 2010; 35(5): 220-4
- Shaw S A. Lee A. Student nurses’ misconceptions of adults with chronic nonmalignant pain. Pain Manag Nurs 2010; 11(1): 2-14
- Doorenbos AZ, et al., A blueprint of pain curriculum across prelicensure health sciences programs: one NIH Pain Consortium Center of Excellence in Pain Education (CoEPE) experience. J Pain 2013: 14(12): 1533-8
- Yannick Tousignant-Laflamme MT, Lussier D, Lebel P, Savoie M, Lalonde L, Choinièere M, Educational needs of Health Care Providers working in Long-Term Care Facilities with regard to pain management. Pain Res Management 2012; 17(5): 341-346
- Watt-Watso, J et al. The ethics of Canadian entry-to-practice pain competencies: how are we doing? Pain Res Manag, 2013; 18(1): 25-32
- IASP. Curriculum Outline on Pain for Nursing. 2012 (cited May 2015); Available from: http://goo.gl/wg4FAH
- Barr HFD, Hammick M, Koppel I, Reeves S. Evaluations of interprofessional education: a United Kingdom review for health and social care. London: United Kingdom Centre for the Advancement of Interprofessional Education with the British Educational Research Association; 2000
- Szasz G. Interprofessional education in the health sciences. A project conducted at the University of British Columbia. Milbank Mem Fund Q 1969; 47(4): 449-75
- Szasz G, Education for the health team. Can J Public Health, 1970; 61(5): 386-90
- Watt-Watson JCJ, Finley A, Watson P, Canadian Pain Society position statement on pain relief. Pain Res Manag 1999; (4): 75-8
- DiCenso A, et al Advanced practice nursing in Canada: overview of a decision support synthesis. Nurs Leadersh (Tor Ont), 2010; 23 Spec No 2010: 15-34
- Musclow SL, Sawhney M, Watt-Watson J. The emerging role of advanced nursing practice in acute pain management throughout Canada. Clin Nurse Spec 2002; 16(2): 63-7
- Fishman SM, et al. Core competencies for pain management: results of an interprofessional consensus summit. Pain Med 2013; 14(7): 971-81
- IASP. Interprofessional Pain Curriculum Outline. 2012 (cited May 2015); Available from: http://goo.gl/BcDNGD
- Lax, L, et al. Innovation and design of a web-based pain education interprofessional resource. Pain Res Manag 2011; 16(6): 427-32.
